Sialendoscopy and Salivary Stones
A Minimally Invasive Diagnostic and Therapeutic Technique
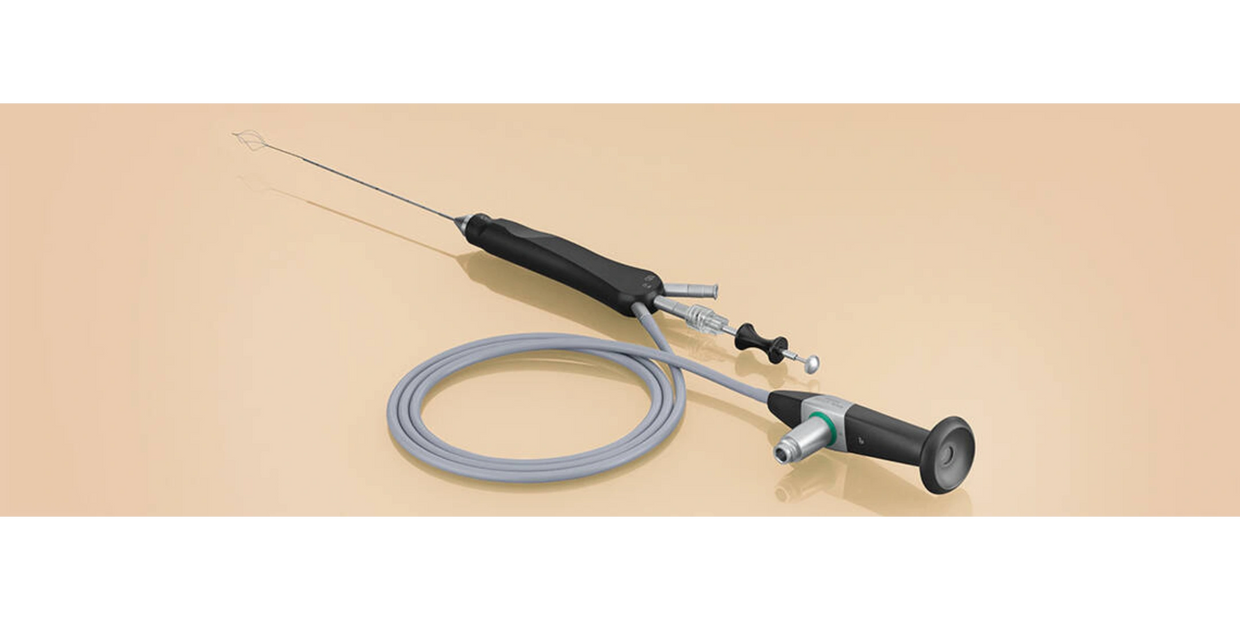
Sialendoscopy is a minimally invasive endoscopic procedure used to diagnose and treat various disorders of the salivary glands, such as salivary gland stones (sialolithotomy), stenosis, and strictures. During the procedure, a small endoscope is inserted into the salivary gland duct to visualize the interior of the duct and remove any obstructions or lesions. Sialendoscopy is typically performed under local anesthesia and can often be done as an outpatient procedure.
Sialendoscopy offers several benefits over traditional surgical approaches, including a lower risk of complications, reduced scarring, and faster recovery time. However, it may not be appropriate for all types of salivary gland disorders or for all patients.
It is important for individuals with salivary gland disorders to discuss their treatment options with a qualified healthcare professional, who can determine the best course of treatment based on the individual's specific needs and medical history.
What are some of the typical symptoms of salivary stones?
Sialolithiasis, or the presence of a salivary gland stone, can cause a variety of symptoms depending on the location and size of the stone.
The most common symptoms of sialolithiasis include:
- Pain or discomfort in the affected gland or area around the gland
- Swelling or enlargement of the affected gland
- Dry mouth or decreased salivary flow
- Infection or inflammation of the gland (sialadenitis)
- Difficulty opening the mouth or difficulty eating
- Foul-tasting discharge from the gland
The symptoms of sialolithiasis may come and go or be persistent, and they can vary in intensity depending on the size and location of the stone. In some cases, the stone may not cause any symptoms at all and may be discovered incidentally during imaging studies or dental exams. If you experience any of the above symptoms, you should see a healthcare provider for further evaluation and management.
What are salivary stones?
Salivary stones are solid concretions that develop within the salivary system, made up of a combination of minerals and organic substances commonly found in saliva, such as calcium phosphate, calcium carbonate, and proteins.
It is difficult to give an exact percentage of salivary stones that are radioopaque because the composition and size of the stones can vary widely. However, studies have suggested that most salivary stones are at least partially radiopaque, meaning they can be visualized on x-rays or other imaging studies. In one study of 390 patients with salivary stones, 85% of the stones were found to be radiopaque on x-rays.(1) Another study of 121 patients found that 95% of the stones were visible on x-rays. (2)
It's important to note that even if a salivary stone is radiolucent and not visible on x-ray, it can still cause symptoms and may require treatment. Radiolucent salivary stones may also be small or poorly calcified, which can make them more difficult to detect on imaging. Other diagnostic tests, such as sialendoscopy or ultrasound, may be used to visualize radiolucent stones and confirm their presence.
What can make you more prone to salivary stone formation?
Several factors can increase an individual's susceptibility to developing salivary stones, including:
- Dehydration: Lack of proper hydration can result in reduced salivary flow, which can contribute to the formation of salivary stones.
- Poor oral hygiene: Poor oral hygiene can lead to the accumulation of bacteria in the mouth, which can cause inflammation and blockage of the salivary glands, increasing the risk of developing stones.
- Medical conditions: Certain medical conditions, such as Sjogren's syndrome, gout, or chronic infections, can cause changes in the composition of saliva, making it more prone to stone formation.
- Medications: Some medications, such as antihistamines and diuretics, can decrease salivary flow and increase the risk of salivary stone formation.
- Structural abnormalities: Structural abnormalities of the salivary glands or ducts, such as strictures or stenosis, can increase the risk of salivary stones.
- Age and gender: Salivary stones are more common in adults, especially those over the age of 40. Men are also more likely than women to develop salivary stones.
- Dietary factors: Certain dietary factors, such as a diet high in sugar or low in calcium, may increase the risk of salivary stone formation.
It's worth noting that in many cases, the exact cause of salivary stone formation is unknown.
How are salivary stones typically diagnosed?
Salivary stones are typically diagnosed based on a combination of patient history, physical examination, and imaging studies. The following are some of the diagnostic methods commonly used to identify salivary stones:
- Medical history: The doctor will ask about your symptoms, including any pain or swelling in the salivary gland area, and any previous episodes of salivary gland problems.
- Physical examination: The doctor will examine the salivary gland area by palpating it to feel for any lumps or swelling. They may also use a flashlight to check for the presence of stones in the ducts.
- Imaging studies: Imaging studies can help to confirm the presence of a salivary stone. CT scans, and ultrasound are commonly used imaging tests. CT scan is also important for ruling out tumors causing ductal obstruction.
- Sialography: Sialography is a specialized imaging test that involves injecting a dye into the salivary gland ducts and taking X-rays. This study is now mostly outdated and most centers do not offer it.
- Diagnostic sialendoscopy: can diagnose obstructive salivary stones that are not apparent on imaging (radiolucent stones) as well as non stone salivary duct narrowings (stenosis). This study can be both diagnostic and therapeutic in select cases.
If a salivary stone is suspected, your doctor may recommend one or more of these diagnostic tests to confirm the diagnosis and determine the appropriate treatment.
What are some of the consequences of untreated salivary stones?
Salivary stones, also known as sialolithiasis, can cause various complications if left untreated. Some of the sequelae of untreated salivary stones include:
- Recurrent infections: When the salivary gland is blocked due to the stone, the saliva accumulates behind the blockage, leading to the growth of bacteria and subsequent infection. If left untreated, this can lead to recurrent infections.
- Abscess formation: A prolonged infection can lead to the formation of an abscess, which is a collection of pus. This can cause pain and swelling in the affected area.
- Obstruction of the salivary duct: The blockage caused by the salivary stone can lead to the obstruction of the salivary duct. This can cause pain, swelling, and difficulty in eating and drinking.
- Chronic inflammation: Untreated salivary stones can cause chronic inflammation of the salivary gland, leading to permanent damage.
- Sialadenitis: Sialadenitis is an inflammation of the salivary gland. It can occur due to a blockage caused by a salivary stone. If left untreated, this can lead to chronic sialadenitis.
It is important to seek medical attention if you suspect that you have a salivary stone to prevent these complications from occurring. Treatment options include medications to increase saliva flow, gland massage, and surgical removal of the stone.
How does size of the salivary stone affect the ability of a surgeon to remove a stone via sialendoscopy?
The maximum size of a submandibular stone that can be removed reliably via sialendoscopy depends on various factors, such as the location, shape, and consistency of the stone, as well as the skill and experience of the surgeon performing the procedure.
In general, sialendoscopy alone can be effective for stones that are less than 8mm in size that are located in the main duct of the parotid or submandibular glands, as larger stones may be more difficult to remove or require additional procedures such as a combined transoral or transcutaneous (through the skin) approach.
It's important to note that the size of the stone alone is not the only determining factor for the success of sialendoscopy, as other factors such as the patient's anatomy and the underlying cause of the stone formation can also affect the outcome. Therefore, the decision of whether to use sialendoscopy or other treatments should be made on a case-by-case basis by an experienced medical professional.
How does location of the salivary stone affect the ability to remove via sialendoscopy?
The location of a submandibular stone can significantly affect its removal via sialendoscopy.
If the stone is located close to the papilla or opening of the duct in the mouth, it may be easier to remove using sialendoscopy. However, if the stone is located deeper in the duct or in a tortuous part of the duct, it may be more challenging to access and remove with sialendoscopy alone. In some cases, the use of additional tools such as baskets or forceps may be required to successfully remove the stone.
Additionally, the location of the stone can also affect the risk of complications during the procedure. Stones located in the proximal part of the duct may be associated with a higher risk of injury to the duct wall or surrounding tissues, while stones located in the distal part of the duct may be associated with a higher risk of salivary duct perforation. Therefore, the location of the stone is an important consideration when determining the most appropriate approach for removal via sialendoscopy.
1. Bodner L, Bar-Ziv J. Radiographic features of salivary gland calculi: a comparative study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84(6):726-729. doi:10.1016/s1079-2104(97)90336-4
2. Marchal F, Dulguerov P, Becker M, Barki G, Disant F, Lehmann W. Specificity of parotid sialography and B-mode ultrasonography in the diagnosis of parotid gland duct obstruction. J Otolaryngol. 1995;24(3):140-145. PMID: 7607274.
What are some of the other indications for sialendoscopy besides stone retrieval?
- Chronic sialadenitis: This refers to the chronic inflammation of the salivary glands, which can cause recurrent swelling, pain, and infections. Sialendoscopy can be used to identify and treat obstructive lesions or strictures that may be causing the inflammation.
Reference: Marchal F, Dulguerov P, Becker M, Barki G, Disant F, Lehmann W. Interventional sialendoscopy. Laryngoscope. 2000;110(2 Pt 1):318-20. doi: 10.1097/00005537-200002000-00029. PMID: 10680865.
- Recurrent sialadenitis: This refers to multiple episodes of acute sialadenitis, which can be caused by a variety of factors such as bacterial infections or autoimmune diseases. Sialendoscopy can help identify and treat the underlying cause of recurrent sialadenitis.
Reference: Otsuka H, Sato Y, Nakamura T, et al. Sialendoscopy-assisted treatment for recurrent parotitis. Auris Nasus Larynx. 2018;45(2):219-223. doi: 10.1016/j.anl.2017.04.009. PMID: 28558934.
- Juvenile recurrent parotitis: This is a type of recurrent sialadenitis that affects children and adolescents. Sialendoscopy can be used to diagnose and treat the underlying cause of the recurrent parotitis, such as ductal obstruction or strictures.
Reference: Katz P, Hartl DM, Guerre A, Périé S, Marchal F. Sialendoscopy in Juvenile Recurrent Parotitis. JAMA Otolaryngol Head Neck Surg. 2018;144(7):622–627. doi:10.1001/jamaoto.2018.0513
- Sjogren's syndrome: This is an autoimmune disorder that affects the salivary glands, causing dry mouth and eyes, as well as other systemic symptoms. Sialendoscopy can be used to identify and treat obstructive lesions or strictures in the salivary ducts, which can contribute to the symptoms of Sjogren's syndrome.
Reference: Del Signore AG, Marchese Ragona R, Antonelli A, et al. Sialendoscopy in patients with Sjogren's syndrome: a systematic review. Acta Otorhinolaryngol Ital. 2020;40(4):249-259. doi:10.14639/0392-100X-N0884. PMID: 32894784.
- Iodine-induced sialadenitis. Radioactive Iodine-131 is used as adjuvant therapy in certain types of thyroid cancer. In addition to uptake in the thyroid tissue, iodine can concentrate in salivary gland tissue and ducts. This can result in pain, swelling, and obstruction of the salivary ducts. Sialendoscopy can be used to identify and remove any obstructive debris within the salivary ducts, and to perform irrigation and suction to remove any residual iodine or inflammatory material. Additionally, steroid injection therapy or the use of anti-inflammatory medications can be administered during the sialendoscopic procedure to help reduce inflammation and promote healing of the salivary glands. Several studies have reported the effectiveness of sialendoscopy in the treatment of iodine-induced sialadenitis. For example, a 2012 study published in the Journal of Oral and Maxillofacial Surgery reported that sialendoscopy was successful in resolving symptoms in 95% of patients with iodine-induced sialadenitis. Early intervention with sialendoscopy is important in the treatment of iodine-induced sialadenitis, as delayed treatment can result in permanent damage to the salivary gland tissue. Therefore, patients experiencing symptoms of post-iodine sialadenitis should seek prompt evaluation and treatment by a specialist experienced in sialendoscopy and salivary gland disorders.
Reference: Lu D, Duan X, Chen X, Chen L, Wang C, Chen Z. Sialendoscopy in the Treatment of Iodine-Induced Sialadenitis. J Oral Maxillofac Surg. 2012;70(1):81-88. doi:10.1016/j.joms.2011.02.059
It is worth noting that sialendoscopy is a relatively new technique, and its indications and efficacy are still being studied and refined. Additionally, the use of sialendoscopy may depend on the individual patient's clinical presentation and underlying pathology. Therefore, it is important to consult with a specialist experienced in sialendoscopy and salivary gland disorders to determine the appropriate course of diagnosis and treatment.
Historical Note:
Salivary endoscopy is a gland sparing procedure for treatment of salivary stones and other obstructive conditions of salivary ducts. Advent of endoscopic techniques has reduced the need for surgery to remove salivary glands (parotidectomy and submandibular glands) for obstructive and inflammatory salivary gland disease.
Copyright © 2023 Saliva M.D. - All Rights Reserved.
Powered by GoDaddy
This website uses cookies.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.